Endodontic Microsurgery: A microscopic surgical procedure indicated when a root canal infection is not healing after non-surgical treatment
What is endodontic microsurgery?
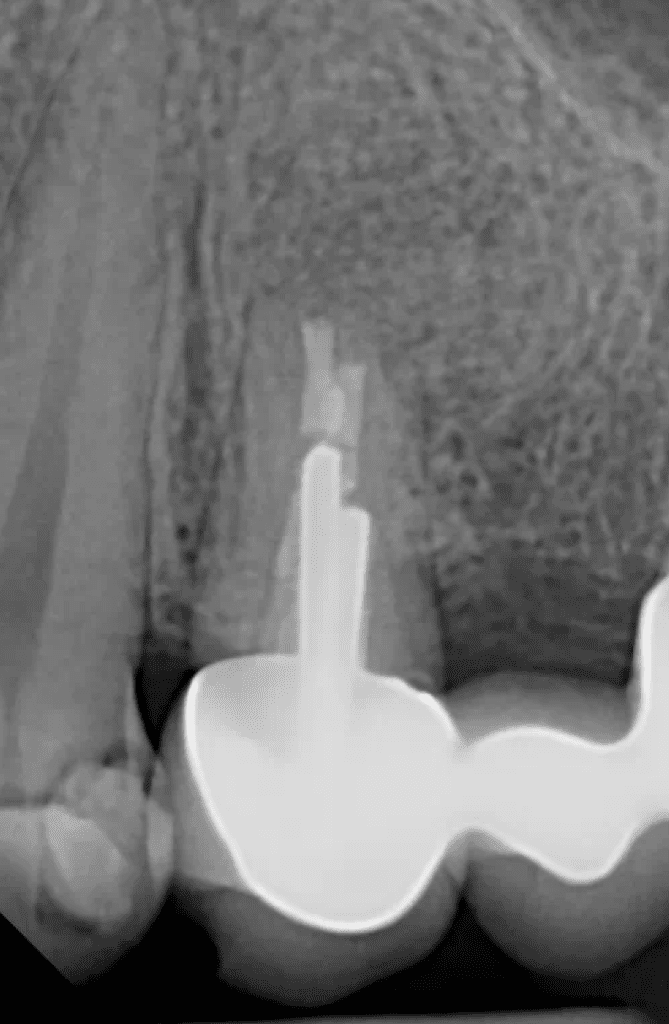
Root canal microsurgery is often indicated when root canal treatment or retreatment is not healing the infection. There are several circumstances when apical microsurgery or an apicoectomy may be indicated. Complex canal anatomy at the tip of the root can result in bacteria that are unable to be reached with a traditional root canal or root canal retreatment. There can also be extra-radicular biofilm (bacteria) on the outside of the root that is unable to be reached with a root canal. Some times there are posts cemented inside of a tooth to help hold the crown in place that we do not want to risk tooth fracture by removing the post for retreatment making endodontic microsurgery the more conservative treatment approach. We use CBCT (3D) imaging for all endodontic microsurgery evaluations to help diagnose the cause for the recurrent infection and guide best treatment options. Dr. Sullivan uses the surgical operating microscope for all endodontic microsurgery procedures. Advanced microsurgical techniques used at Mason Endodontics and Microsurgery ensure less post-operative discomfort, a maximized rate of success, and faster healing times.
1st Step of Endodontic Microsurgery
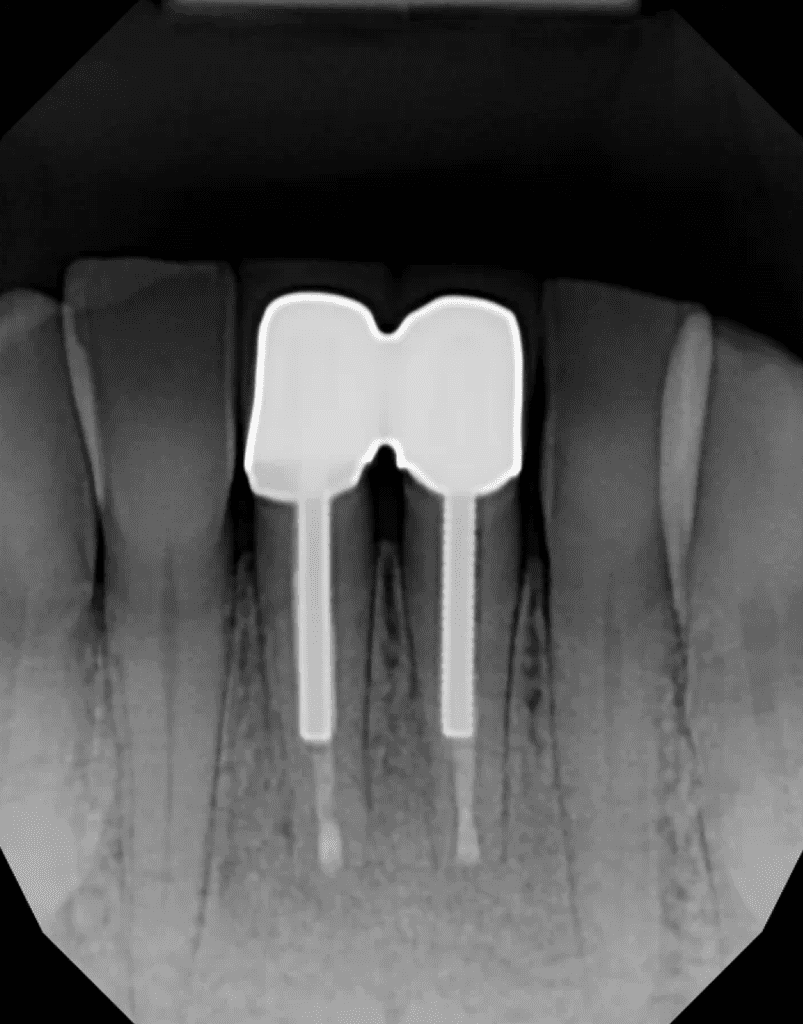
The surgery is planned out on the CBCT (3D) imaging software. We measure the length of your root and make a plan to resect or remove 3 mm of the tip of the root. Endodontic literature shows that removing 3 mm of the end of the root gets rid of the majority of complex canal anatomy in the tip of the root that bacteria can be hiding in. Our digital treatment planning approach ensures precise and safe treatment. Any questions you may have are answered and consent forms are reviewed prior to the date of surgery due to oral sedation often being used on the day of the procedure to reduce anxiety and increase comfort. If oral sedation is utilized, you must have a driver to and from the appointment on the date of the surgery.
2nd Step of Endodontic Microsurgery
Oral sedation medication is often prescribed and taken 1 hour prior to the appointment. You will swish around an antibacterial mouth rinse for 60 seconds. A small incision is made along the gum line and the gum is gently lifted to expose the root of the tooth that is infected. The tip of the root is removed as well as any infected tissue. We create a small retro-preparation in the canal of the tooth to remove approximately 3 mm of previous root canal filling material and any bacteria inside the tip of the canal. A biocompatible filling material, MTA, is placed into the canal space to provide a seal and prevent reinfection. The entire procedure is completed through the microscope for the highest success rate.
3rd Step of Endodontic Microsurgery
The surgical site is irrigated very well with saline throughout the procedure to keep everything clean. A bone graft and resorbable collagen membrane is some times recommended depending on the amount of bone loss to encourage complete regeneration of the bone that was lost due to the infection. The gum tissue is gently placed back into its original position and sutures are placed. Pressure is held for 10 minutes.
Final Step of Endodontic Microsurgery
Dr. Sullivan will review all post-operative instructions including the recommended medication protocol. A post-operative report with x-rays is sent to your general dentist. We see you back at our office in 3 to 7 days to remove the sutures and check healing. The sutures are removed and you are scheduled back for a 6-month healing check to make sure the area is healing well and that the infection has resolved.
How do I know if I may need endodontic microsurgery?
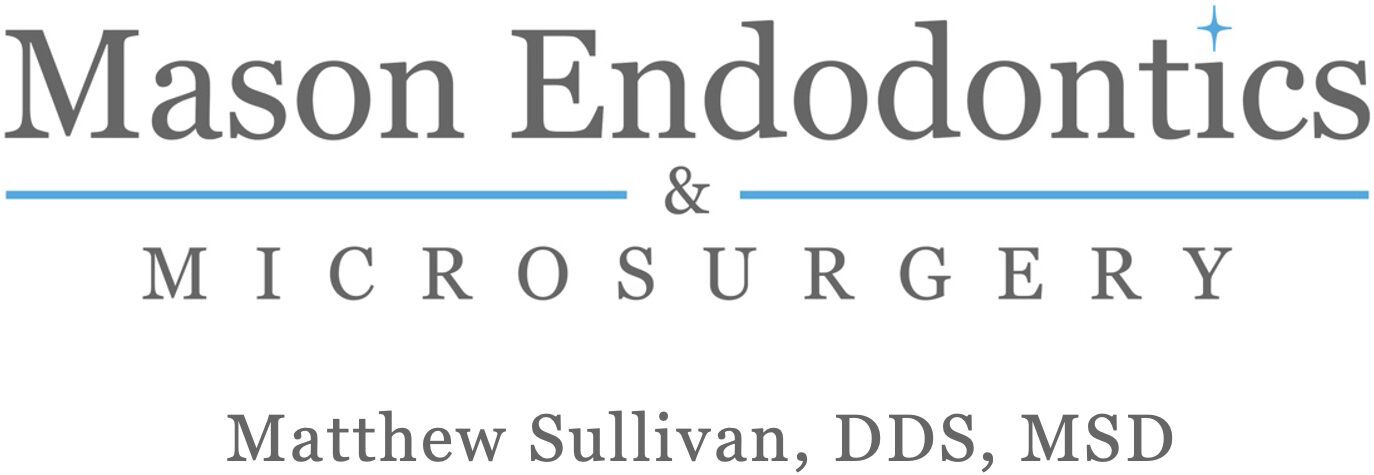
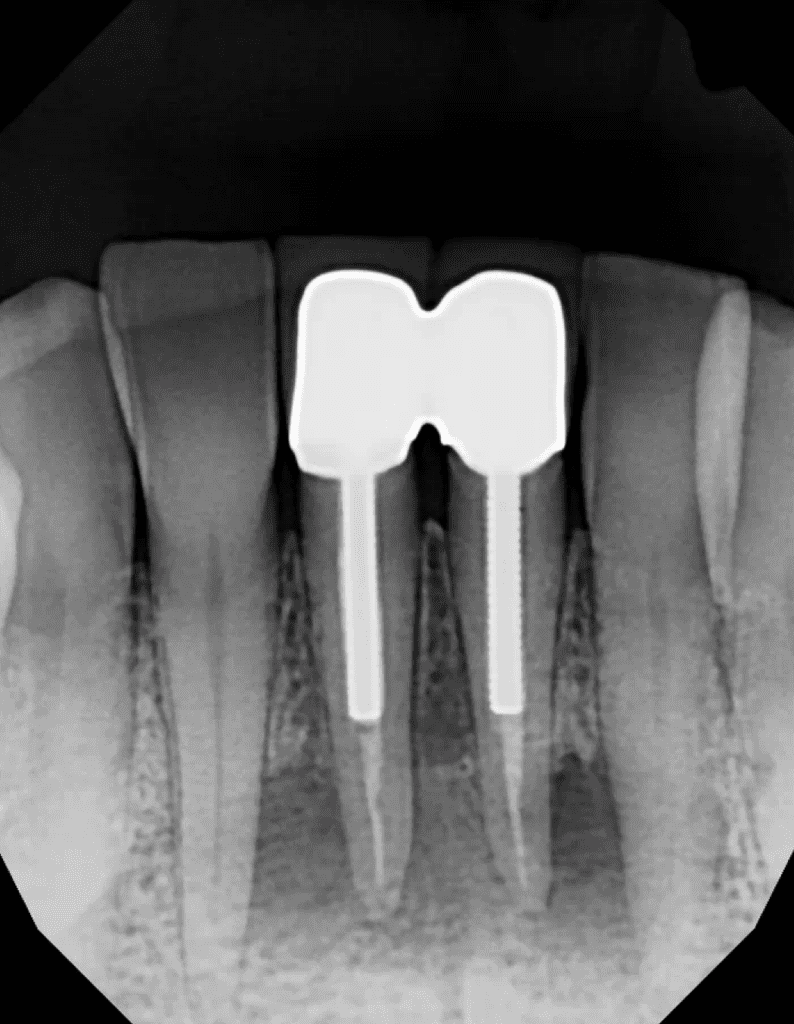
-Your dentist may find a periapical radiolucency (shadow) on an x-ray of a previously root canal treated tooth
-Non healing of an infection after root canal treatment
-Tenderness to palpation (touch) of the roots of a tooth after root canal treatment
-Pain when chewing your food
-Spontaneous throbbing or aching from your tooth or jaw
-Pain that wakes you up at night or that you have to take medications to relieve
-Trauma to a tooth that causes fracture or the tooth to be loose
-A small bump, swelling, or “pimple” next to a tooth or more severe swelling in the jaw or cheek
-Persistent sinus issues on one side can be a sign of tooth infection